Introduction
The global prevalence of obesity among adults has steadily risen from 4.6% in 1980 to 14.0% in 2019 [1]. South Korea was no exception to this global trend. According to the 2023 Obesity Fact Sheet, the overall obesity prevalence in 2021 increased to 38.4% from 30.2% in 2012, representing a 1.27-fold increase. Specifically, the prevalence of class II to III obesity exhibited significant increases from 0.35% (men) and 0.42% (women) in 2012 to 1.21% and 0.97% in 2021, respectively, indicating rises of 3.46-fold and 2.31-fold [2]. For patients with Class II to III obesity classified by body mass index (BMI)—where Class II is defined as a BMI between 35.0 and 39.9 kg/m² and Class III is defined as a BMI of 40.0 kg/m² or higher—the prevalence of type 2 diabetes mellitus (T2DM) is reported to be as high as 40% (95% CI, 32.1–48.3). This increased risk is attributed to factors such as insulin resistance and excessive obesity [3]. Once T2DM develops, patients face challenges including increased cardiovascular risk, nerve damage, and potential complications affecting organs such as the kidneys and eyes [4-6]. Predicting and early managing T2DM In class II to III obese patients is crucial for mitigating risks and improving overall health outcomes [7]. Implementing comprehensive strategies from the onset can significantly enhance treatment efficacy and patient prognosis [7].
Obesity is a chronic condition that requires a multidisciplinary approach encompassing lifestyle improvements such as pharmacological and surgical treatments, dietary and physical activity modifications, emotional support, and mental health management [8]. In this multidisciplinary approach, the focus is not only on weight management in severely obese patients but also on preventing and early detecting complications [8]. The multidisciplinary team in bariatric services includes bariatric physicians, dietitians, clinical psychologists, surgeons, physiologists, and nurses [9]. Nurses play a key role as providers of specialized medical or surgical clinical care, conducting clinical assessments, education, and patient treatment. Within these centers, the role of nurses in patient education and counseling is becoming increasingly important [10, 11]. Specifically, there is a need for nurses to provide patients with straightforward yet effective education on the risk of developing T2DM, particularly in preventing and early detecting T2DM in severely obese patients based on multidimensional clinical evidence [12]. Therefore, this study aimed to explore the potential of utilizing anthropometric parameters, obtainable through fundamental body measurements, to predict the risk of T2DM.
Methods
1. Study Participants
This study analyzed data from 72 severely obese patients who participated in the main Korean obesity surgical treatment study (KOBESS), a multicenter, single-arm study [13]. The ethical approval and all cohort protocols of the KOBESS trial can be found in the protocol paper [14]. The approval number of the coordinating investigator is INHA 2016-06-015. In this cohort data, the analyzed data for this study included eligible participants if they had BMI of ≥35 kg/m².
2. Measures
Anthropometric measurements were conducted using the Quad Scan 4000 multi-frequency bioelectrical impedance analyzer from BodyStat®, UK. Based on these measurements, the waist-to-hip ratio (WHR), body roundness index (BRI), and a body Shape index (ASBI) were calculated using the following formulas. ASBI, waist circumference/(BMI2/3 × height1/2); BRI, 364.2 − 365.5 × {1 − [(waist circumference/2π)/(0.5 × height)]2}1/2; WHR, waist circumference/hip circumference × 100 [15].
For serum analysis, patients fasted for 8 hours before sampling, which was used to measure fasting blood glucose (FBS), HbA1c, and the lipid profile. T2DM was characterized by an FBS level of ≥126 mg/dL and an HbA1c level of ≥6.5 % [16]. Patients taking antidiabetic medications were categorized into the T2DM group, regardless of meeting diagnostic criteria.
3. Statistical Analyses
The characteristics of participants were compared between groups based on the presence of T2DM using the Mann-Whitney test for continuous variables and the Pearson chi-square test for categorical variables. Logistic regression models were generated to investigate the associations between anthropometric parameters and T2DM. Areas under the receiver operating characteristic curve (AUC) were calculated to assess the performance of individual parameters in predicting T2DM.
Statistical analyses were performed using SPSS 23.0 software (IBM SPSS, Inc., Chicago, IL, USA). Statistical significance was determined at a 5% alpha level (95% confidence interval) with 80% power. A p-value < 0.05 was considered statistically significant.
Results
1. Baseline characteristics
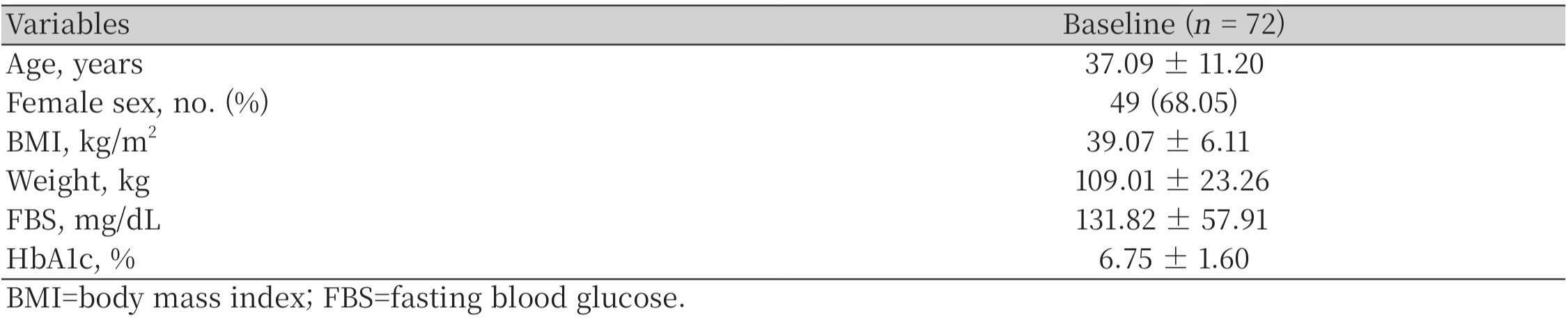
This study involved 72 participants, with an average age of 37.09 ± 11.20 years. Among them, 49 participants were female, comprising 68.05% of the total sample. The mean BMI was 39.07 ± 6.11 kg/m², and the average body weight was 109.01 ± 23.26 kg. Participants had an average FBS level of 131.82 ± 57.91 mg/dL and an average HbA1c level of 6.75 ± 1.60% (Table 1).
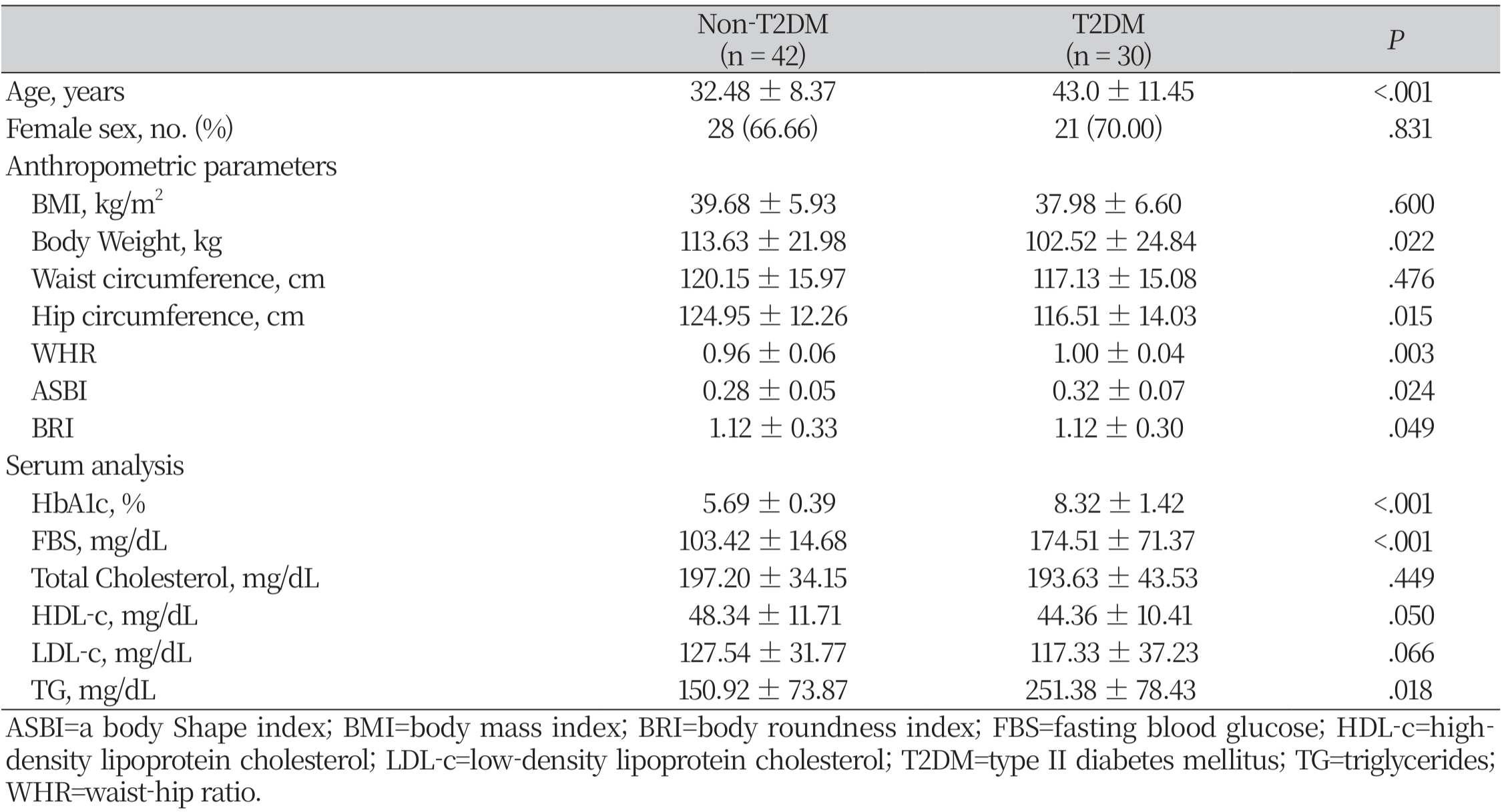
2. Differences in anthropometric parameters and serum analysis between non-T2DM and T2DM groups
The general characteristics and anthropometric parameters according to the serum levels of HbA1c are in Table 2. Significant differences between the non-T2DM and T2DM groups were observed in anthropometric variables, including body weight (p = .022), hip circumference (p = .015), WHR (p = .003), ASBI (p = .024), and BRI (p = .049). In serum analysis, significant differences were observed in HbA1c (p< .001) and FBS (p< .001), as well as in HDL (p = .050) and TG (p = .018).
3. Predictors for T2DM In class II to III obese patients
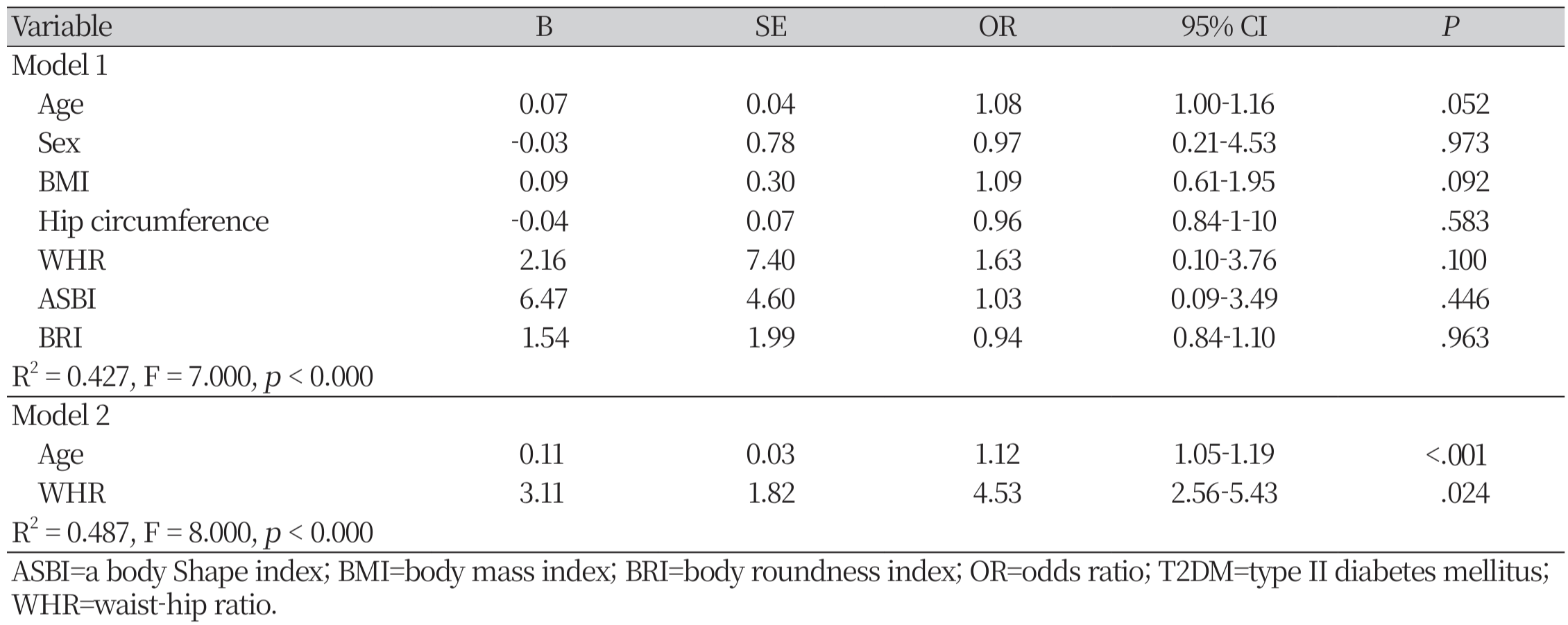
Unadjusted outcomes for T2DM prediction are presented in Model 1, showing: age (p = .052), sex (p = .973), BMI (p = .092), hip circumference (p = .583), WHR (p = .100), ASBI (p = .446), and BRI (p = .963). In Model 2, adjustments were made, revealing significant predictors of T2DM: age (p< .001; OR, 1.12; 95% CI, 1.05 – 1.19) and WHR (p = .024; OR, 3.11; 95% CI, 2.56 – 5.43) (Table 3).
ROC curves were generated using age and WHR, variables that showed significant associations with predicting T2DM in obese patients. Age and WHR demonstrated superior performance in predicting T2DM among obese patients. The AUC for age was 0.794 (p< .000; 95% CI 0.56 – 0.85), and for WHR it was 0.721 (p = .003; 95% CI 0.39 – 0.69) (Figure. 1).
Discussion
This study focused on exploring the utility of anthropometric parameters derived from basic body measurements in predicting the risk of T2DM among class II to III obese patients. Our results underscored significant differences in anthropometric variables such as body weight, hip circumference, BRI, ASBI, and WHR between non-T2DM and T2DM groups. These parameters, along with serum biomarkers including HbA1c, FBS, HDL-c, and TG, provided critical insights into the metabolic profile associated with T2DM risk. Studies investigating the correlation between increases in body weight, BMI, and waist circumference with an increased risk of T2DM have been widespread in the general population, yielding somewhat consistent results [16, 17]. However, research on the correlation between these variables and T2DM in obese populations is relatively limited, and the results are inconsistent [18-20].
According to our research analyzing patients with class II to III obesity, age and WHR were identified as predictors of T2DM. The association between age and T2DM risk corroborates previous epidemiological evidence highlighting age as a non-modifiable risk factor [21, 22]. Meanwhile, WHR, reflecting central adiposity, demonstrated a significant association with T2DM independent of age and other variables. WHR evaluates how fat is distributed between the waist and hips, with higher WHR indicating more central obesity [23], which is associated with increased overall health risks compared to obesity where fat accumulates more around the hips and thighs [24, 25]. Therefore, the analysis of WHR through anthropometric measurements in patients classified as class II to III, along with the assessment of T2DM risk based on body shape, is deemed clinically useful. The use of age and WHR in combination yielded promising predictive performance, as evidenced by the AUC values of 0.79 and 0.72, respectively.
This study's findings contribute to supporting the importance of anthropometric measurements in clinical settings, particularly highlighting that while weight and BMI are primary variables in identifying individuals at high risk for T2DM in the general population [21, 22], in patients with class II to III obesity, measurements reflecting central obesity, rather than overall weight, are more crucial. The integration of these straightforward yet effective measures into routine clinical practice, coupled with comprehensive multidisciplinary care, holds promise for enhancing early detection and prevention efforts in managing obesityrelated metabolic disorders.
Conclusion
In conclusion, utilizing WHR, a body measurement parameter reflecting central obesity, along with age provides a practical approach to predicting T2DM risk in class II to III obese patients. Future research should further explore the utility of these measurements and consider additional biomarkers to enhance prediction models, ultimately optimizing personalized interventions to alleviate the burden of T2DM in this vulnerable population.